Covid 19 Ethics Resources
I started to develop this page at the beginning of the pandemic when information resources were scattered and few. I updated it until the summer of 2020 and have decided to archive it as many of the links are still useful. The government very unhelpfully migrated much C19 guidance during 2020, so the links to official government guidance no longer work. Most others remain current.

Ethical decisions are made all the time in health care, but the Covid 19 pandemic is posing some unfamiliar questions. This page shares key resources that groups or individuals may find useful. It includes links to official policy, professional guidance and selected research. You can navigate directly to each section via the headings below.
- Guidance from NHS, NICE, GMC & Royal Colleges
- Governance and strategy for leaders & ethics forums
- Duties of care to staff
- Caring for ethnically diverse patient groups
- Mental health law, disability and human rights
- Caring for the deceased
(This page focuses on advice and guidance from UK professional and official bodies and includes a few significant academic publications. The UK Clinical Ethics Network and Nuffield Council on Bioethics have pages with a wider remit and range of media.)
Thank you to @DrCicely and @JonathanIves4 who started me off by putting me onto very welcome resources.
Professional body & official guidance
- The General Medical Council has collated specific advice on dealing with ethical challenges associated with Covid19 in a series of FAQs. These address key concerns including inadequate PPE.
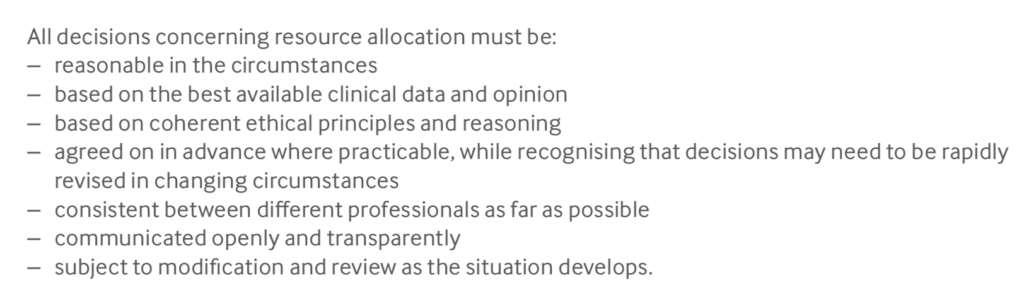
- A collaborative of medical Royal Colleges has published ethical guidance, reviewed by GMC and hosted by the Royal College of Physicians. See Ethical Dimensions of Covid19 for Front Line Staff. It makes an important statement regarding fairness in decisions surrounding escalation of care:
- The BMA has also published guidance for doctors Covid19 – ethical issues which builds upon the ethical principles for pandemic influenza revised by the DHSC in 2017 (see below). On resource allocation, it states
- NICE has several times updated its COVID-19 rapid guideline: critical care which now includes the role of specialists in assessing frailty and includes a one page critical care admission algorithm. (Thanks to Priya Singh at GSTT for the link). This is the key national guidance for ensuring that access to critical care gives most benefit to those who need it, and that it is allocated fairly and consistently.
- Following news that groups of elderly, frail and chronically ill patients have been asked to complete DNAR forms irrespective of individual circumstances, the CQC, BMA, RCGP and Care Providers Association have issued a joint statement making clear that this practice is unacceptable.
-
The Royal College of Nursing has published guidance on DNACPR emphasising the importance of individualised decision making in discussion with patients or their representatives.
- The Intensive Care Society has stated on its website:
“In particular, on the topic of potential ‘triage by resource’ (declining a patient on the basis of capacity rather than the usual triage by likely outcome/benefit), the following apply:
> External: nobody should triage until everybody triages (which should be a national decision). We are a networked service and until the last bed in the last hospital is occupied, there are always options.
> Internal: no one should make capacity-related admission decisions alone. Trust systems such as ‘three wise people’ should be deployed for mutual multidisciplinary support.
- Giving unwelcome news with compassion and clarity is practical ethics in action. Health Education England has a comprehensive range of resources freely available on its e-learning for health website. It includes an evidence based framework for communicating unwelcome news, and a checklist for doing this by phone.
- The Royal College of Psychiatrists has a developing suite of resources including a summary of ethical issues and principles, emergency amendments to MHA 1983, risk stratification in community mental health, and remote consultations. Emergency legislation in the Coronavirus Act introduces significant changes to the Mental Health Act (NOT YET IN FORCE). These include changes to rules on length of detention, formal admission, and administration of medication without consent.
- The Royal College of General Practitioners has published responses to a number of ethical questions of particular salience in primary care, and linking to other sources of guidance.
- NHS England recently published this important guide to caring for people with learning disability or autism (or both) during the outbreak. It notes that “in 2018/19 at least 41% of people with a learning disability who died, died as a result of a respiratory condition. There is therefore, strong reason to suspect that people with a learning disability may be significantly impacted by the coronavirus pandemic.” The guidance is directed at clinicians who may have limited experience of managing the care of this group of patients.
- The British Geriatric Society has published guidance Managing the Covid19 pandemic in care homes. It has notable ethical reminders around visiting, alternatives to restraint for residents who ‘walk with purpose’ (wander), the need for advance care planning, being clear why admission to hospital may be apt or inapt, and accepting residents back on discharge from hospital.
- Resuscitation Council UK provides as needed updates on its Statements on COVID-19 in relation to CPR and resuscitation It also has a useful guide for lay people about the need to have conversations in advance about care in a health crisis, explaining how the ReSPECT process helps patients to make wishes known.
- This NHSE guidance on palliative care during Covid19 has helpful reminders on approaching end of life care with compassion for patients and their families. Includes a simple ‘three talk model’ for shared decision making. See Clinical guide for the management of palliative care in hospital during the coronavirus pandemic – Keeping the care in healthcare
- Statement by the Faculty of Forensic and Legal Medicine on the imperative of fulfilling the duty of care to patients in police custody.
- Joint statement by the health professions regulators on expectations of practice during the pandemic https://www.gmc-uk.org/news/news-archive/how-we-will-continue-to-regulate-in-light-of-novel-coronavirus
Governance and strategy for leaders & ethics forums
- The UK Clinical Ethics Network which supports clinical ethics committees (CECs) now has a regularly updated page on its website giving access to Covid ethics resources and assistance to CECs. It has links to external resources including academic and international commentary.
- The DHSC document ‘Responding to Covid 19: an ethical framework for adult social care’ sets out principles that are equally relevant to providers of mental and community health services. It sets out eight principles: Respect; Reasonableness; Minimising harm; Inclusiveness; Accountability; Flexibility; Proportionality; and Community. It states Respect and Reasonableness are fundamental, and that otherwise the principles carry equal weight.
- In 2017 the Department of Health published a revised ethical framework for pandemic influenza planning, tweaking one developed in 2007. It appears to have informed the 2020 DHSC ethical framework for adult social care (see above). The ethical framework can be found within this longer document.
- Information Governance. NHSX has published guidance on information governance during Covid19, including provision for sharing patient information for public health purposes.
- The Hastings Centre (US) has issued a useful guide to strategic ethical considerations, PDF here and at The Hastings Centre
- Will providers or clinical staff face potential legal liability for non standard care under pandemic conditions? This statement from NHS Employers explains how the Clinical Negligence Scheme for Trusts will continue to indemnify staff.
- The Nuffield Council on Bioethics (UK) policy briefing emphasises “People should be treated as moral equals, worthy of respect. While individuals may be asked to make sacrifices for the public good, the respect due to individuals should never be forgotten” and “Solidarity is crucial at the international level between countries, by businesses in how they exercise their corporate social responsibility; and at the individual level in the way we all respond to the outbreak in day-to-day life.”
Duties of care to staff
- A helpful brief article in Journal of Medical Ethics discussed ethical considerations in deploying staff to higher risk areas. The authors consider allocation by volunteering, by lottery, and sharing risk by assigning all staff to high risk duties through rota design. None is perfect.
- An important article by Greenberg and others in BMJ addresses minimising moral injury in care staff during Covid19. Key messages: managers need to proactively take steps to protect the mental wellbeing of staff; must be frank about the situations staff are likely to face; support staff by reinforcing teams and providing regular contact to discuss decisions and check on wellbeing; once the crisis begins to recede, actively monitor, support and where necessary offer treatment to staff. Importantly, they advise that “Single session psychological debriefing approaches should not be used as they may cause additional harm”.
- The Intensive Care Society UK maintains a well being resource library. This includes an incredibly informative poster on understanding staff well being over a period of crisis, and another great poster on self care for staff. Great advice on how to look after yourself and others, relevant to all staff (including managers), not just intensivists.
- Research article by Ives et. al. Healthcare workers’ attitudes to working during pandemic influenza: a qualitative study (Open Access) The researchers asked staff what would motivate them to go or not go to work. In summary, it is worth paying attention to the following factors (besides staff being ill themselves). Practical aspects: caring responsibilities (children, spouse, parents etc) and whether a substitute carer can be found or provided; perceived level or risk to self & also to those for whom there are caring responsibilities; transport availability, particularly when less transport is running and for night shifts; availability of appropriate personal protective equipment; availability of on-site or near-site accommodation. Psychological factors Staff anxiety about having to make rationing decisions and adapt treatment protocols, with their fear of subsequent litigation exacerbated by lack of authoritative guidance; positive motivating factors of loyalty to team, professionalism, being useful; and an expectation of reciprocity – if I put myself out for others, will I be looked after by the organisation?
Caring for ethnically diverse patient groups
- It is now clear that people from BAME backgrounds are disproportionately affected by Covid19. Among many reasons, one is that they are not receiving information in their first language. Doctors of the World has translated the NHS Coronavirus information into 45 different languages in downloadable PDFs.
Mental health law, disability rights, human rights
- Coronavirus and the Mental Capacity Act. A thoughtful blog on the implications of the MCA 2005 in pandemic circumstances, when large numbers of people who may lack capacity to consent require urgent treatment.
- Mental Capacity Law and Policy is a web page maintained by leading barrister Alex Ruck-Keene. It currently (26th March) contains pretty much all that is anticipated about how the Coronavirus Act 2020 will affect duties owed under the Mental Capacity Act. Note that the Coronavirus Act changes will not come into effect until triggered by order.
- Disability, coronavirus, and international human rights. This web page is maintained by Doughty Street Chambers to promote the interests of all people with disabilities, including cognitive disability and mental ill health. Links to UN and WHO sources, and draws attention to need to consider people with disabilities in prison.
- Advance decision resources for individuals. Many people expect that their partners or family members will be asked to make decisions about their care when they are too ill to do so. In law, that is not the case – those close should be consulted, but they will not have the final say. However, individuals can make a binding advance decision or give power of attorney to another person to make decisions. Charity Compassion in Dying helps people through the process with structured information, forms and a helpline.
Caring for the deceased
How can the dead be truly dead when they still live in the souls of those who are left behind? (Carson McCullers)
- New national guidance on caring for the deceased with sensitivity dignity and respect, and for protecting mourners and service providers from Covid19 infection.